 Here we go again. New plague. Same stigma. Gay and bisexual men have been told they cannot donate their plasma to a trial hoping to provide a treatment for COVID-19.
Here we go again. New plague. Same stigma. Gay and bisexual men have been told they cannot donate their plasma to a trial hoping to provide a treatment for COVID-19.
To be clear this is not about access to treatment. It merely reinforces a discriminatory provision already in place for blood donation. Men who have sex with men cannot donate blood if they have engaged in sexual activity in the last three months.
Until 2011, when a time limit of 12 months was introduced, gay and bisexual men were banned from donating altogether. Twelve months became three in 2018. But the underlying prejudice is the same.
I’m 59, no more or less high-minded than the next citizen. Though if anything my sense of social responsibility has been enhanced by my sexuality. But I haven’t given blood since I was 24. Never mind that like all donated blood mine would be screened. It is unwanted.
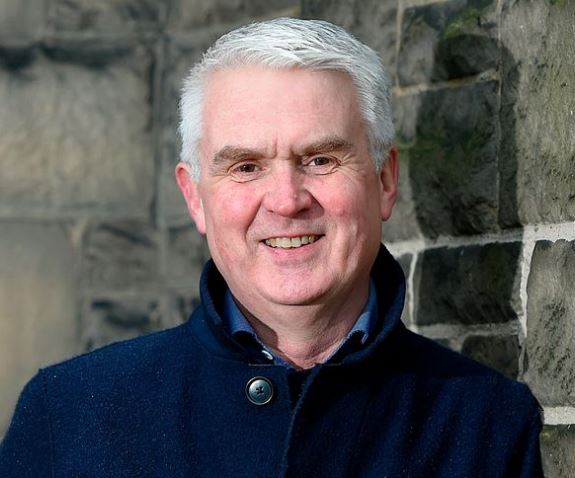
There was something especially poignant about this story emerging as the news broke of Derek Ogg’s untimely death. In the days when hysteria about the gay plague whipped up homophobia, “people like Ogg made Scotland a more tolerant country long before it was fashionable” wrote Bernard Ponsonby.
I was in London back then and never met Ogg, but I had known of him for more than 30 years. In the 1980s, we happy few who campaigned for gay rights heard of each other one way or another.
And just when we could see light ahead, we were thrown into darkness by the arrival of AIDS. Our efforts turned to public information campaigning as others whose job it was sat on their hands or worse, resorted to scare tactics.
I have already written that for those of us who lived through that crisis, it has proved impossible not to pick at the scab it left behind these past few weeks. You can be forgiven for thinking it healed a long time ago.
But emotional scars don’t. For my generation of gay men and the one which preceded it, the devastation wrought by HIV upturned our world. Its shadow is unending.
I have been in rooms of gay men caught in that shade. It hurts. Still.
Maggie O’Farrell, whose recently published novel, Hamnet, is set against the recurrence of the Black Death, recently reflected that perhaps, in coping with COVID-19, we are looking to ingrained history lessons about the plague.
For us, those lessons are very recent. The new virus in our midst is not the same as HIV. Yet the public discourse it has spawned is replete with resonance. We trip over it daily.
The lexicon of COVID-19 is one of relentless parallels. AIDS framed our world. There is nothing new about testing. The language of antibodies, of positive and negative, is one we have long lived with.
We watch stories about fears that PPE is not available for those who need it and remember the panic that led to it being used by those who didn’t.
It is no surprise to us that death registration is not as neat as headline writers would like. My late partner’s death certificate makes no mention of HIV or AIDS. He died of the thing that got him in the end — ‘chronic dementing illness.’
We are all too familiar with fears, real or imagined, about touching dead and dying bodies. We recall Princess Diana holding that dying man’s hand. I remember the limits placed on how long my late partner’s coffin could be open when he came home to rest the day before his funeral.
And for masks, read condoms. No matter they have other health benefits, we had no choice but to use them. AIDS turned sex into something dangerous, just as COVID-19 turns has turned everyday sociability into a hazard. Masks are barriers too; however necessary they might prove to be.
And then there’s ‘the peak’, perhaps the cruellest parallel. My partner died in 1995, the year AIDS deaths peaked in the UK. I didn’t know it at the time. Nor that if he could have lived just another 12 months, he might even have been alive today.
But to blood again. It’s instructive to cast our minds back.
The virus we now know as HIV wasn’t named until 1986. There was no antibody test until the year before. Even then, its reliability was a work in progress. But there was no mistaking the mounting death toll.
False positives and negatives, uncertainty about time frames — science took time to become more exacting. The associated anxiety was woven into the fabric of our lives.
It is worth remembering too the focus of early efforts to develop an HIV antibody test. It was not on preventing the spread of the virus among those most at risk but on screening donated blood.
And yet we know, tragically, lives were lost. In the UK, 1,243 people with haemophilia became infected with HIV of whom less than 250 are still alive.
How many of those deaths were avoidable is a moot point. We know it took too long for the government to accept the mounting medical evidence that the virus could be transmitted by blood products.
The report of the Penrose Inquiry into Hepatitis C/HIV acquired infection from NHS treatment in Scotland with blood and blood products makes sobering reading.
At one point, in late 1983, a courier travelling from Paris to London with a flask of virus arrived at Waterloo late after ferry and train delays. There was no one to meet him and he had to leave it in a lock-up where it died.
A witness to the inquiry estimated six months were lost in terms of the epidemiology. He could only look back and weep. “We might have had a British isolate, a UK isolate, much earlier”, had that not happened he said. The language sounds horribly familiar, doesn’t it?
It is impossible to conclude that blood which led to the loss of lives did not come from gay men. The virus ripped through our community. And it remains true that gay men are at higher risk of contracting HIV.
But since the rules were amended in 2018, Stonewall has continued to call for a system based on individualised risk assessment of blood donors, rather than complete exclusion.
As the plasma story broke, Laura Russell, the charity’s policy director, responded, “It’s really upsetting that gay and bisexual men who want to help in the fight against coronavirus are being prevented from doing so.”
How right she is. Back then, as the virus came and the response of science unfolded falteringly, we were in the eye of the storm. Our lovers were dying. Yet we, and they, were at the vanguard of halting its spread.
We found ourselves the recipients of marginalisation and bile, not large-scale state aid. Now as the unceasing impact of COVID-19 reminds us every day — and in every way — of the long road to survival, we are caught short again.
After all these years, ours is still bad blood. It needn’t be this way. Stigma isn’t healthy, nor inevitable. History has a lesson for those who want to learn.